More than 650,000 Ohioans have lost their Medicaid coverage since the COVID-19 public health emergency ended, according to data from KFF.
During the federal public health emergency, states received extra funding for Medicaid. In exchange, they paused their disenrollments. The number of Medicaid recipients in Ohio rose to more than three million in early 2023. That’s a million more people than just three years prior.
But that pandemic provision ended last April, launching a review of all enrollees’ eligibility and the start of the Medicaid “unwinding” process – a euphemism for kicking people off its rolls.
Hailey Akah, vice president of operations and strategy at the Health Policy Institute of Ohio, said the process has impacted access to healthcare throughout the state.
“There's many, many more Ohioans today that don't have insurance coverage potentially than did a year ago,” Akah said. “Without access to affordable insurance coverage, people are more likely to delay care, which means health conditions get worse.”
Ohio’s Medicaid population
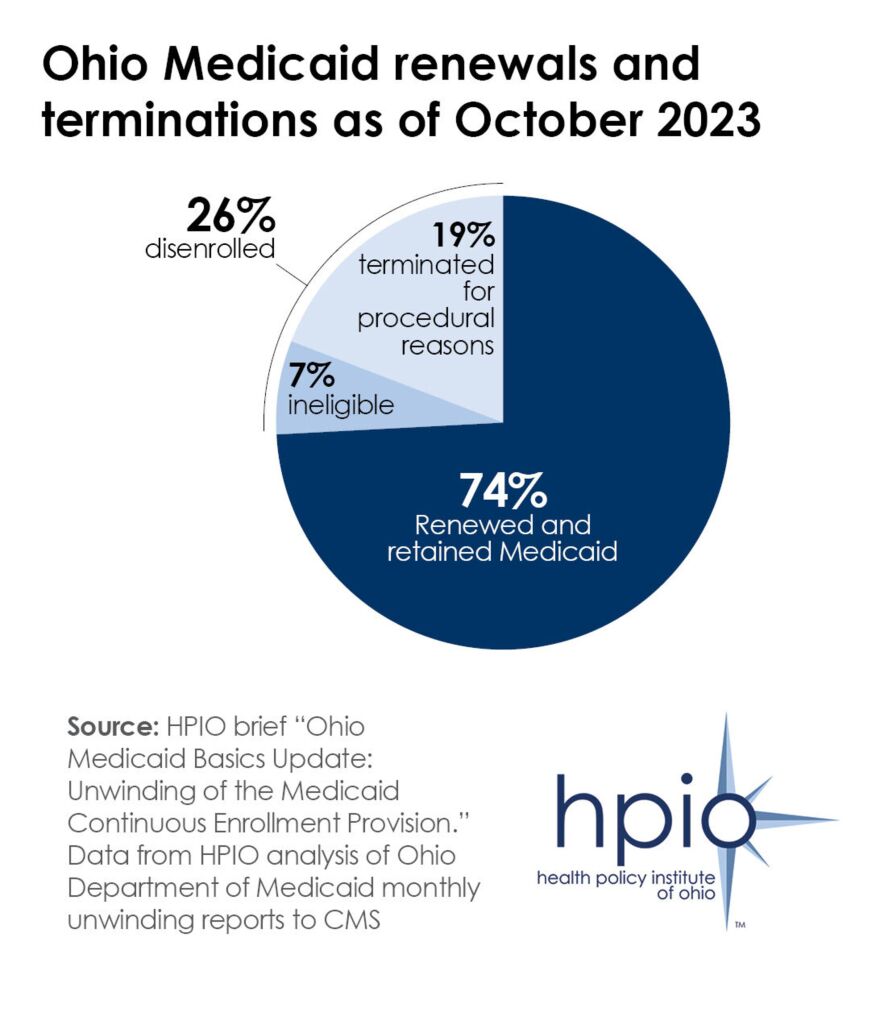
Akah said while a large number of Ohioans have lost their health insurance coverage, they’re not in the majority. Around three-fourths of Ohioans who had their eligibility reviewed have maintained coverage.
Nationally, more than 17 million Medicaid recipients have been deemed ineligible for Medicaid insurance. Akah said, compared to many other states, Ohio has done well in continuing enrollment.
“Ohio has the 11th lowest rate of disenrollment, meaning most states in the nation have disenrolled people at a higher rate than Ohioans,” Akah said.
Ohio is one of the top Medicaid spenders in the nation, ranking sixth, according to KFF. In fiscal year 2022, the state spent $30 billion on Medicaid.
A wide variety of people can be eligible for Medicaid – low-income adults, children and families, people with disabilities and older adults. Akah said the state has seen disenrollment across all categories.
And, Akah said enrollees have been taken off the rolls for different reasons. Some may have gained employer health insurance, or seen their financial situations change and are now ineligible. The majority of Ohioans who have been removed during the redetermination process are for procedural reasons, like an incorrect address or outdated contact information. But, Akah said a good portion of those people were likely ineligible anyway.
“Ohio sort of mirrors the national rate for procedural disenrollment, so it's kind of on par with other states there,” Akah said.
Rebuilding coverage
The state’s Medicaid unwinding process is expected to come to an end this month, and Akah said it’s essential that every Ohioan can have access to affordable healthcare.
Akah said those who were kicked off for procedural reasons may need assistance in re-enrolling. For those deemed ineligible for Medicaid, they may apply for subsidized coverage through the federal health insurance marketplace.
“There have been policy changes at the federal level that have opened up additional subsidies for coverage on the marketplace,” Akah said. “So people who are currently without coverage, after being disenrolled from Medicaid, can check healthcare.gov to see if they're eligible for one of those subsidies.”
Get Covered Ohio, led by the Ohio Association of Foodbanks, is helping Ohioans explore other health insurance options and complete necessary forms to gain coverage.
Akah said it will be awhile before the state fully understands the impact of the disenrollments.
“We'll just have to wait and see how the system works,” Akah said.


